News and blogs
205 articles
 Blog
BlogMichael Holland sets the analogue to digital vision
Our chief executive Michael Holland recently presented an opening talk at the annual Cavendish Square Group Conference
 News
NewsSupporting children’s mental health through art
Our creative art therapy service is an accessible and inclusive form of therapy, which uses creative expression as a tool for understanding emotional growth.
 News
NewsStrengthening community CAMHS across North Central London: A new collaborative approach
We’re pleased to share an important update about the future of Community Child and Adolescent Mental Health Services (CAMHS)
 News
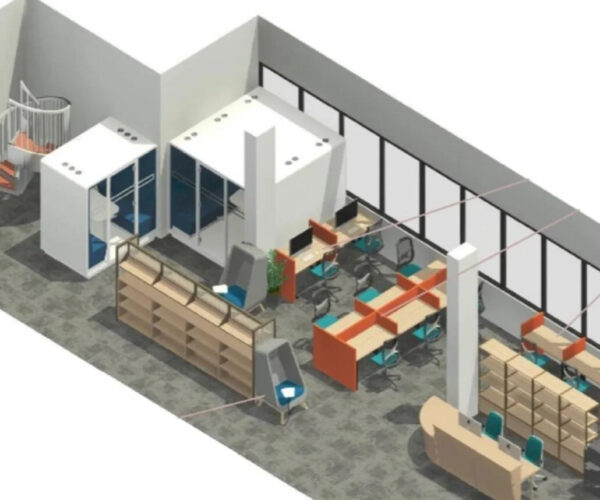
NewsTavistock Centre library summer closure
We’re closing our spaces to make big improvements ready for the new academic year
 News
NewsReceive appointment reminders via our patient portal
Patients at our gender identity clinic (GIC) can now receive appointment notifications and reminders through our patient portal.
 News
NewsStudent uses manga art to express emotions in their studies
A student has been using manga art to help express emotions from their studies and therapy sessions.
 News
NewsSupporting parents and children through our family drug and alcohol court (FDAC) service
Our family drug and alcohol court (FDAC) service hosted a showcase event
 Blog
BlogRelational practice in our Camden adolescent intensive support service
Maintaining a safe and robust crisis service through ‘Relational Practice’ in an Adolescent Intensive Outreach Support Service
 News
NewsTavistock and Portman student receives Royal College of Nursing Foundation award
Student recognised in the Royal College of Nursing (RCN) Foundation Impact Awards.
 News
NewsGloucester House introduces pet therapy
Gloucester House, our Trust-run school, has been working with the national charity Pets as Therapy (PAT) to enhance the health and wellbeing of their students.
 News
NewsTavistock Consulting at 30: Videos of celebratory event
Recordings from an event celebrating 30 years of consultancy practice.
 News
NewsTavistock and Portman NHS Foundation Trust merger update
Update on Tavistock and Portman NHS Foundation Trust merger plans.
 News
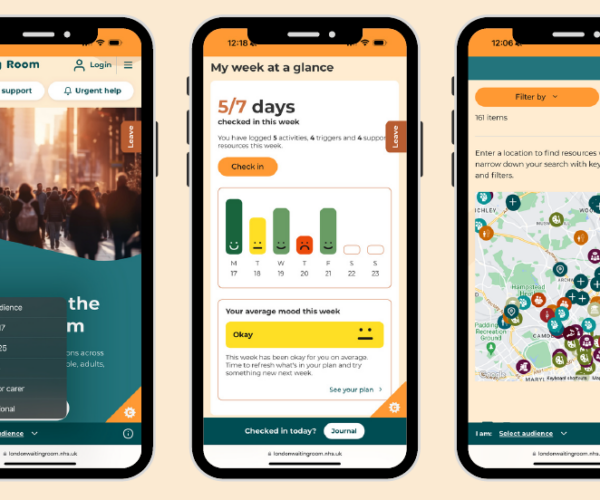
NewsWaiting Room relaunches with new features and support options
Showcasing a variety of health and wellbeing services for people of all ages across London.
 News
NewsWaiting Room shortlisted for HSJ Digital Awards
Our Waiting Room has been shortlisted in the ‘Improving Mental Health through Digital’ category.
 News
NewsCelebrating 30 years of Tavistock Consulting
Tavistock Consulting is our specialist organisational development and change consultancy
 News
NewsNotice of Council of Governors elections 2025
Notice is hereby given that elections will be held for the Council of Governors for The Tavistock and Portman NHS Foundation Trust.
 News
NewsSupporting autistic children at risk of harming others: Conference February 2025
We welcomed an array of professionals from across the UK to our FCAMHS Conference on Thursday 13 February.
 News
NewsCelebrating Mental Health Nurses Day
Mental Health Nurses Day encourages us to celebrate the incredible work of mental health nurses.
 News
NewsFebruary 2025 open day
We were delighted to welcome aspiring postgraduate students to our on-site open day on Saturday 1 February 2025.
 News
NewsThree tips to help children express emotions
Adi Steiner shares guidance on how to facilitate conversions about difficult things with children and young people
 News
News2024 publishing successes
Browse some of the articles, chapters and books published by our staff, students and alumni over the past twelve months.
 News
NewsCamden mental health support team for schools showcased in NHS England Medical Director visit
Dr Adrian James visited our Camden mental health support team.
 News
NewsSupporting Camden foster carers through a monthly support group
How our Growing with you CAMHS service supports foster carers.
 News
NewsReady to kickstart a new career in 2025?
Join our in-person open day on Saturday 1 February 2025 to get a real taste of student life at The Tavistock and Portman.
